
The sharp rise in Sepsis DRG coding and reimbursement has emerged as one of the most prevalent billing challenges facing health plans today.
Each one of these cases requires anywhere from 1-3 hours of painstaking manual review, causing costly bottlenecks. Clinical documentation of septic patients is non-standard and often lacks the level of specificity needed for accurate DRG assignment, making errors all too common. And with ever-evolving clinical criteria and coding requirements, regulatory compliance remains an ongoing challenge.
Sepsis DRGs represent some of the highest-cost episodes in healthcare, with reimbursement rates that are often 2-3 times higher than standard infection codes. Between overpayments and added administrative burden, sepsis upcoding is costing payers billions of dollars annually.
At Alaffa, we’re using AI to build the solution.
Sizing the Sepsis Upcoding Problem
Financial impact: In 2019, the HHS Office of Inspector General (OIG) found that Medicare spent $7.4 billion on septicemia or severe sepsis with major complications (DRG 871), the most frequently billed diagnosis.1 By 2023, that number had risen to over $8.2 billion.2
Rising sepsis diagnoses: An HHS study found that the rate of Medicare beneficiaries hospitalized with sepsis increased by 40% from 2012 to 2018, nearly double the rate of Medicare enrollment growth.3 This dramatic increase, occurring while mortality rates remained stable, suggests that coding practices rather than true disease prevalence are driving the growth.
Vulnerable billing patterns: Of the roughly 3.5 million stays billed at the highest severity level, nearly 1 million lasted a "particularly short amount of time", equating to a 20% shorter length of stay than the mean for the assigned diagnosis code).4 The OIG noted that "although the complications billed suggest sicker beneficiaries, the shorter lengths of stay point to beneficiaries who are less sick," indicating potential upcoding.5
Audit burden: Health plans spend millions annually on retrospective chart reviews, with sepsis audits taking 60-180 minutes per chart and requiring specialized clinical expertise to evaluate subtle documentation nuances.
Provider abrasion: Aggressive sepsis audits with limited rationale or explanation strain provider relationships, with physicians frustrated by subjective clinical and coding criteria and inconsistent audit standards across different payers.
Meeting the Moment with Agentic AI
Built on manual processes and reactive auditing, traditional approaches to payment integrity can no longer meet the complexity and volume of modern health insurance claims. But with the rise of AI-native solutions, health plans finally have the tools to bend the cost curve.
Agentic AI represents the future: systems that understand clinical nuance, apply complex coding rules at scale, and continuously improve. This amplifies and enables clinical teams to work at the top of their license, focusing their time and attention where it matters most while the AI agents handle routine work.
For healthcare payers struggling with sepsis upcoding, the question is no longer whether they should adopt AI-powered solutions, but how quickly they can implement them: to protect payment integrity, reduce costs, and strengthen provider relationships.
Our Sepsis DRG Validation Solution
At Alaffia, we’re using cutting-edge AI to transform Sepsis DRG reviews with a consistent, objective, data-driven approach that replaces slow, subjective manual validation. Built on advanced machine learning, payer policy frameworks, and up-to-date, evidence-based clinical criteria that evolve with the latest definitions, our technology standardizes sepsis detection and classification across every case, streamlining reviews and driving faster, smarter outcomes.
Here’s how it works.
1. Configuration
We configure our DRG agent to meet your clinical needs, with your plan’s specific data, policies, and processes integrated into our AI platform to create bespoke workflows and outputs. This ensures that we adhere to your audit process requirements.
2. Data extraction
Comprehensive medical records spanning admission to discharge are normalized into pre-built clinical facts to flexibly service your clinical decisioning needs, then annotated by our clinicians for accuracy.
3. Documentation analysis
The agent cross-references the normalized patient medical records against your clinical criteria and policy guidelines to evaluate whether documentation supports sepsis as defined by your configuration.
4. Smart triage
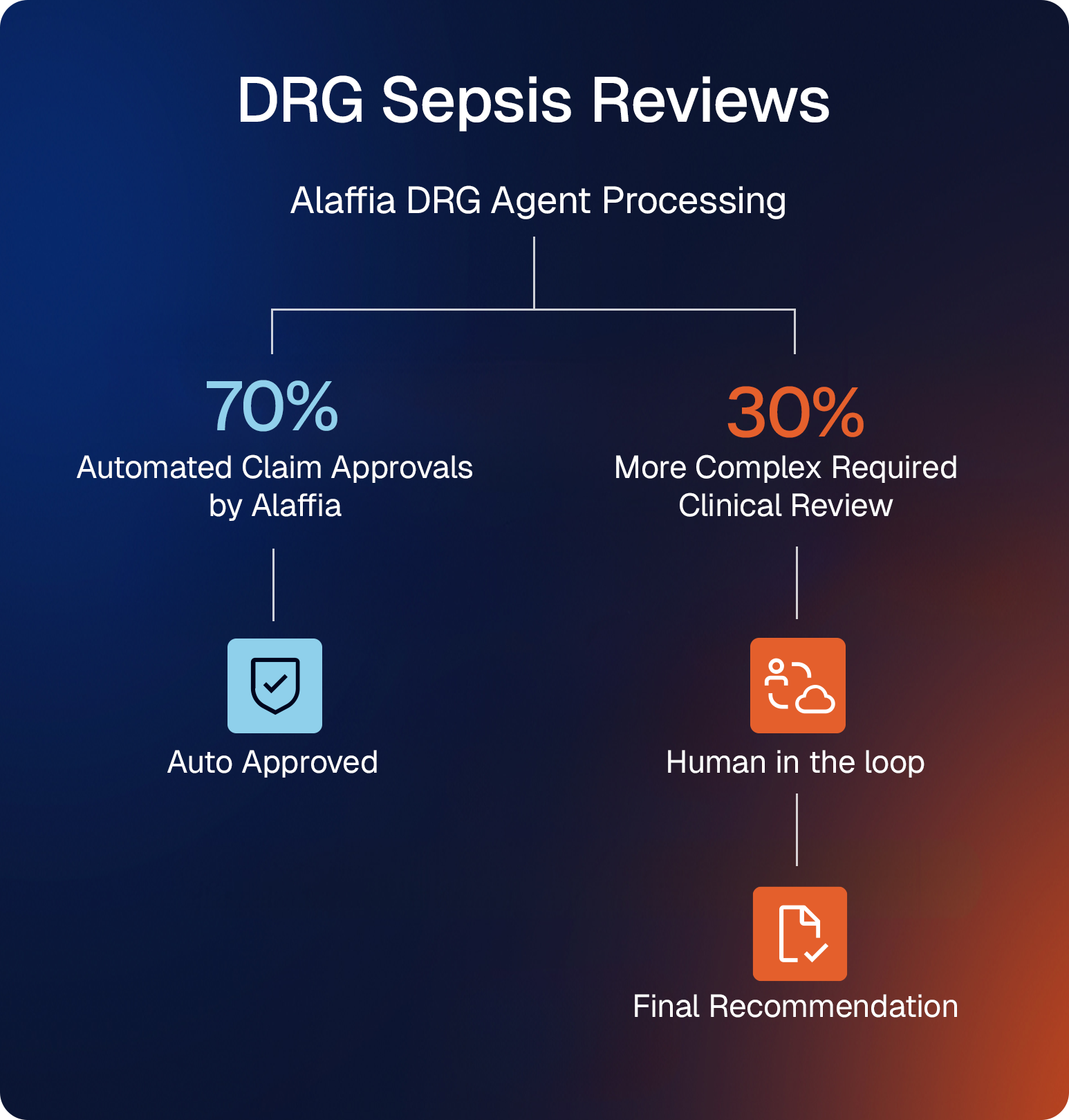
The agent pre-processes all sepsis cases, automating the 70% of reviews that are correctly coded by the provider and routing the remaining 30% (high-value cases that require human review) to your clinicians.
5. Human validation
Every recommendation includes a clear clinical rationale and traceable source citations, with links back to the original medical records and policy documents for verification. Human clinicians are always at the helm for overview and signoff.
With Alaffia, payers gain confidence in every decision.
The Alaffia AI Advantage
Our sepsis DRG validation solution represents a paradigm shift in how healthcare payers approach sepsis upcoding.
Speed and scalability
With our sepsis DRG agent analyzing claims, you can reduce manual review time by 80% and handle growing case volumes without proportional increases in staffing.
Accuracy and consistency
AI agents apply coding criteria uniformly across all claims, ensuring proper DRG assignment and eliminating the variability inherent in manual reviews conducted by different auditors.
Cost efficiency
By automating the review process, especially data extraction, health plans can achieve 60-70% cost reduction compared to traditional approaches while increasing review coverage.
Provider partnership
Our platform automatically drafts clear rationale letters backed by policies and guidelines, helping providers improve coding quality and fostering collaboration rather than conflict.
This is a powerful, transparent, and defensible validation process that aligns with payer policies, eliminates bias, and ensures accuracy at scale. But our technology isn’t the only thing that sets Alaffia apart: the expertise behind it does, too.
Our clinical team is made up of certified billers and coders with decades of experience, and our clinicians (RNs and MDs) have backgrounds in patient care: they understand how codes are generated and how hospital departments work. These SMEs work hand-in-hand with our engineers and AI researchers on the development of our platform, providing crucial real-world perspective that ensures the technology we build is made to work on the ground.
Future-Proof Your Plan with Alaffia
At Alaffia, we’ve saved our health plan partners $100M and counting. While implementation can take months or even years with legacy vendors, we get up and running in just 30 days — driving immediate ROI with no disruption to operations.
Contact us today to learn how our AI-powered solution can help you:
- Automate 70% of routine sepsis reviews
- Reduce improper sepsis payments by 30%+
- Improve documentation quality across your provider network
- Achieve rapid ROI with minimal implementation burden
The sepsis upcoding crisis demands a new approach. Alaffia delivers it.
Drive health plan affordability with Alaffia
Find out what our AI agents and managed services can do for your plan.





